You are stressed. Will your skin be stressed too? If yes, how will it show?
Not a wall!
Once upon a time, people thought of their skin as an inert “wall” that could be polished and would glow. Wrong! Think of the skin as a complex organ that contains neuronal networks, linked to the rest of the body also via blood vessels and lymphatic vessels. Ignore the skin complexity and vitality at your own risk.
Stress
Psychological stress arises when people are under mental, physical, or emotional pressure. It happens when we perceive that pressure exceeds our adaptive power. The brain perceives stress and stress hormones such as corticotropin-releasing hormone (CRH), glucocorticoids, and epinephrine are released, triggering a wide range of physiological and behavioral changes and responses that try to adapt the body to stress. If the stress responses are inadequate or excessive, they may trigger adverse physiological events. Research shows that stress can trigger and/or exacerbate multiple conditions, including cardiovascular disease, asthma, migraine, and neurodegeneration. But we already knew that, right?
The skin is both an immediate stress perceiver and a target of stress responses.
Skin and the consequences of stress
The skin is constantly self-remodeling itself, and modifying cells and mini-organs like the hair follicle and sebaceous glands. It is also a place where the immunological machinery is involved in inflammation and immune defense; and a factory of growth factors, vasoactive chemicals, and hormones.
The skin, a self-regulating protective barrier organ, has sensory and computing capabilities that help counteract the environmental stressors, maintaining and restoring disrupted cutaneous homeostasis. The skin’s complex functions are coordinated by a cutaneous neuroendocrine system that also communicates bidirectionally with the central nervous, endocrine, and immune systems, all acting in concert to control body homeostasis.
The relationship between brain and skin goes both ways because the flow of information goes both ways.
- Skin disease (like chronic inflammation or acne) will lead to stress: reactive depression, adjustment disorder, an anxiety disorder.
- The direction “stress to skin” leads to delusional parasitosis and body dysmorphic disorder.
- Often, the interaction goes both ways, like in atopic dermatitis, psoriasis, acne, etc. where stress will worsen the skin problem and vice versa.
The mechanism
Stress activates the response systems through the hypothalamus-pituitary-adrenal axis (HPA), then the Sympathetic axis (SA), the Cholinergic axis (CA), and finally neuropeptides and neurotrophins. These processes are very complicated, but maybe some examples will help.
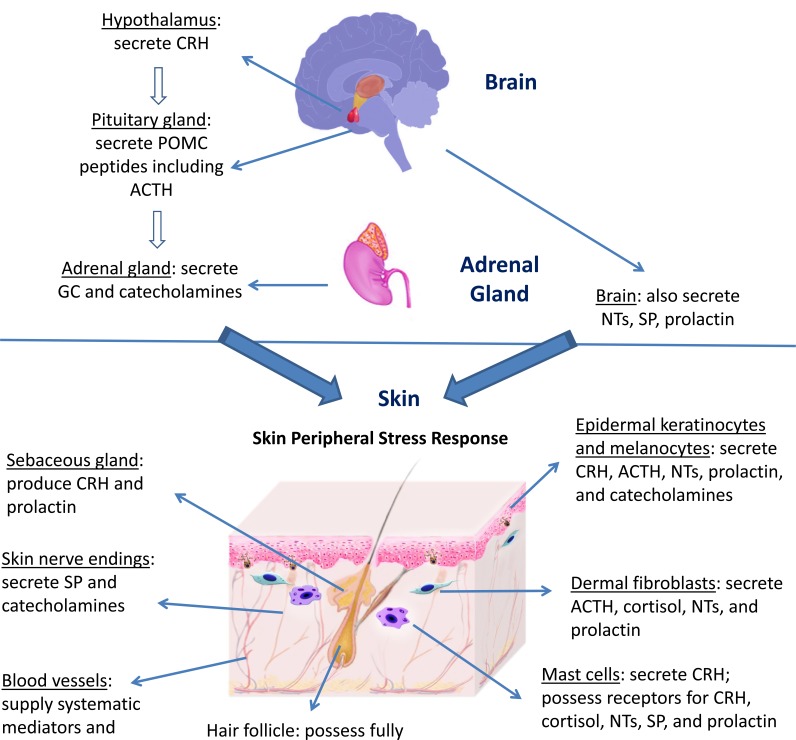
Figure: Central stress response and skin peripheral stress response. From Chen Y, Lyga J. Brain-skin connection: stress, inflammation and skin aging. Inflamm Allergy Drug Targets. 2014;13(3):177-190. doi:10.2174/1871528113666140522104422
Acne
Acne causes anguish, no doubt about that, and we also worry about the likelihood of acne-related problems like skin picking, secondary infection, scarring, post-inflammatory hyperpigmentation, and acne recurrence. There is less information about how the other direction works, but it seems that anxiety and stress in professional and personal life, increase acne frequency and intensity. Researchers have found a relationship between stress and acne flare-ups. In response to stress, our bodies produce more androgens, and these hormones stimulate the oil glands and hair follicles in the skin, which promore acne.
There is increasing evidence that the sebaceous gland expresses receptors for several neuropeptides and is involved in responses to stress. Among them, corticotropin-releasing hormone (CRH) was currently found to be produced also in the skin. The sebaceous gland exhibits an independent peripheral endocrine function and expresses receptors for neuropeptides. Previous reports have confirmed the presence of a complete corticotropin-releasing hormone (CRH) system in human sebocytes in vitro. The capability of hypothalamic CRH to induce lipid synthesis, induce steroidogenesis and interact with testosterone and growth hormone suggests that it may be involved in the development of acne.
Healing
Psychological stress adversely affects the immune system. Peripheral-blood leucocytes in people under stress produce significantly less interleukin-1 beta mRNA in response to lipopolysaccharide stimulation that controls cells. Psychological stress has measurable effects on proinflammatory cytokine production in the local wound environment. Stress-related defects in wound repair could have important clinical implications, for instance for recovery from surgery.
Psoriasis
Psoriasis is a chronic skin inflammatory disease, characterized by overproliferation of keratinocytes and inflammation, which lead to epidermal hyperplasia, dysregulated angiogenesis, skin infiltrating T lymphocyte, and expression of proinflammatory T helper (Th) 1 cytokines. Although recent research has revealed parts of the pathogenesis and the intricate crosstalk between nerves, immune system, endocrine system, and skin cells, these advances have not produced a cure for psoriasis.
Stress exacerbates psoriasis. The pro-inflammatory cytokines that are highly expressed in psoriasis are potent activators of the hypothalamus-pituitary-adrenal axis. This could lead to a vicious cycle and amplify the negative effects. Stress leads to a hyporesponsive central HPA axis with blunted cortisol response and upregulation of inflammatory cytokines. In psoriasis stress also has an impact on the skin’s peripheral HPA axis, and the sympathetic-adrenal medullary (SAM) axis.
Atopic Dermatitis
Atopic dermatitis (AD) is a chronic and relapsing inflammatory skin disease often associated with eczema and itching. Skin barrier function defect is a key feature of AD because null mutations in the filaggrin gene are an important predisposing factor for AD. Environmental factors such as allergens or microbial organisms are critical triggers or complications in the disease. Stress can impact AD symptoms through different mechanisms. Stress can negatively affect the skin’s permeability barrier function and homeostasis. In atopic dermatitis patients, skin barrier dysfunction could lead to increased sensitization to allergens and microbial organisms, increased transepidermal water loss, and a lower threshold for itching.
Similar to psoriasis, atopic dermatitis symptoms and psychological stress seem to form a vicious cycle. AD patients have been reported to have anxiety and depression, while psychological stress exacerbates AD pathology.
Skin aging
Skin aging is characterized by the formation of lines and wrinkles, increased pigmentation, loss of elasticity and firmness, and slower healing. Skin aging is a consequence of both intrinsic factors and extrinsic factors. Environmental stress, including UV light and pollution, leads to DNA, lipid, and protein damage, inflammation, and free radical formation, with all its consequences.
Epinephrine, norepinephrine, and cortisol were found to increase DNA damage, interfere with DNA repair, and alter transcriptional regulation of the cell cycle. It’s interesting that UV irradiation, which is a very direct aging agent, also stimulates the skin’s hypothalamic-pituitary-adrenal axis. UV induces the expression of corticotropin-releasing hormone, proopiome-lanocortin (POMC) peptides, adrenocorticotropin (ACTH), cortisol, and β-endorphin.
And now, for the good news! CBD
The skin is one of the many organs that is equipped with the endocannabinoid system. You may have heard about anandamine. Discovered by Rapahel Mechoulam in 1992, this is one great detective story. If humans have receptors for cannabinoids, CB1, and CB2, there has to be a natural chemical that binds to those receptors. Mechoulam and his coworkers found and characterized that natural chemical, anandamide. 2-arachidonoylglycerol is another natural ligand.
It happens that the skin also has receptors for anandamide. There is not much we can do to increase our endogenous anandamide levels, although chocolate contains chemicals resembling anandamide and I have no doubt that chocolate helps. The good news is that cannabidiol (CBD) is now allowed in skincare products and CBD could help with some skin problems. Let me tell you why.
The cannabinoid signaling extends to the skin and is involved in the maintenance of skin homeostasis, barrier formation, and regeneration. Disruption of the cutaneous cannabinoid system may be involved in several skin diseases and disorders, like atopic dermatitis, psoriasis, scleroderma, acne, hair loss, pigmentation disorders, keratin diseases, and itch.
All of this research is relatively new so we should keep our eyes open for future confirmation (or reversals). In the meantime, let’s take with caution the assertion that anandamide may be linked to hypertrophic scars. The endogenous cannabinoids and say, with confidence, that they are involved in pain and itch.
Fortunately, we now are able to add cannabidiol topically and “top-up” our skin endogenous cannabinoids, for when we need them most. Example: when the skin hurts or itches. I personally, have ELS with CBD on my desk and bathroom and apply it to itchy scars and skin. From what I read, I expect some extra benefits, like faster healing and increased immune competence.
I wonder if that mystery of why we love to be in the sun even when we know that it’s bad for us has to do with endocannabinoids. In fact, UV affects every aspect of the skin which is a complex neuroendocrine system that also communicates with the central nervous, endocrine, and immune systems.
Good news, bad news: although the FDA allows CBD to be used in topical products, banks are a bit behind and block accounts of companies that sell this type of product. We will have to wait until the banking system starts accepting that CBD is a good idea when it comes to skin itch.
References
Glaser R, Kiecolt-Glaser JK, Marucha PT, MacCallum RC, Laskowski BF, Malarkey WB. Stress-related changes in proinflammatory cytokine production in wounds. Arch Gen Psychiatry. 1999;56:450–456.
Bíró, T., Tóth, B. I., Haskó, G., Paus, R., & Pacher, P. (2009). The endocannabinoid system of the skin in health and disease: novel perspectives and therapeutic opportunities. Trends in Pharmacological Sciences, 30(8), 411–420. doi:10.1016/j.tips.2009.05.004
Tóth, K., Ádám, D., Bíró, T., Oláh, A., 2019. Cannabinoid Signaling in the Skin: Therapeutic Potential of the “C(ut)annabinoid” System. Molecules. doi:10.3390/molecules24050918
Peters EM, Liezmann C, Klapp BF, Kruse J. The neuroimmune connection interferes with tissue regeneration and chronic inflammatory disease in the skin. Ann N Y Acad Sci 2012; 1262: 118–26
Rohleder N. Acute and chronic stress-induced changes in sensitivity of peripheral inflammatory pathways to the signals of multiple stress systems – 2011 Curt Richter Award Winner. Psychoneuroendocrinology 2012; 37: 307–16.
Dhabhar FS. Psychological stress and immunoprotection versus immunopathology in the skin. Clin Dermatol 2013; 31: 18–30.
Madva EN, Granstein RD. Nerve-derived transmitters including peptides influence cutaneous immunology. Brain Behav Immun 2013; 34: 1–10.
Rodriguez-Vallecillo E, Woodbury-Fariña MA. Dermatological manifestations of stress in normal and psychiatric populations. Psychiatr Clin North Am. 2014;37(4):625–651
Garg A, Chren MM, Sands LP, et al. Psychological stress perturbs epidermal permeability barrier homeostasis: implications for the pathogenesis of stress-associated skin disorders. Arch Dermatol. 2001;137:53–59
Chiu A, Chon SY, Kimball AB. The response of skin disease to stress: changes in the severity of acne vulgaris as affected by examination stress. Arch Dermatol. 2003;139(7):897–900.
Ganceviciene R, Graziene V, Fimmel S, et al. Involvement of the corticotropin-releasing hormone system in the pathogenesis of acne vulgaris. Br J Dermatol. 2009;160:345–352
Kiecolt-Glaser JK, Marucha PT, Malarkey WB, Mercado AM, Glaser R. Slowing of wound healing by psychological stress. Lancet. 1995;346:1194–1196.
Krause K, Schnitger A, Fimmel S, Glass E, Zouboulis CC. Corticotropin-releasing hormone skin signaling is receptor-mediated and is predominant in the sebaceous glands. Horm Metab Res. 2007;39(2):166–170.
Chen Y, Lyga J. Brain-skin connection: stress, inflammation and skin aging. Inflamm Allergy Drug Targets. 2014;13(3):177-190. doi:10.2174/1871528113666140522104422
DISCLAIMER: These claims have not been evaluated by the FDA and are not intended to diagnose, cure, treat or prevent any disease.