The skin makes and uses vitamin D. See how.
We make vitamin D and we may need vitamin D supplementation. Why? By definition, a vitamin is something we, humans, need to acquire because we can’t make it, but we can produce vitamin D. Why, then, vitamin D supplementation? Because to be able to make vitamin D we need two things: 7-dehydrocholesterol and expose our skin to UVB radiation.
Vitamin D: not only for the bones
Vitamin D has a significant role in calcium homeostasis and metabolism and is crucial for bone formation. Vitamin D influences the bones, but also intestines, immune and cardiovascular systems, pancreas, muscles, brain, and the control of cell cycles. And the skin.
Vitamin D synthesis involves the skin (and liver and kidneys!)
Vitamin D is a fat-soluble vitamin that acts as a steroid hormone and can be synthesized only by a photochemical process. In humans, the primary source of vitamin D is the UVB-induced conversion of 7-dehydrocholesterol to vitamin D in the skin. A whole-body exposure to UVB radiation inducing the light pink color of the minimal erythema dose for 15–20 min is able to induce the production of up to 10,000 IU vitamin D. In the epidermis, vitamin D production is greatest in the basal and spinous layers. Do you see the problem? Whole-body exposure, 15-20 minutes, is not something we get every day in city life.
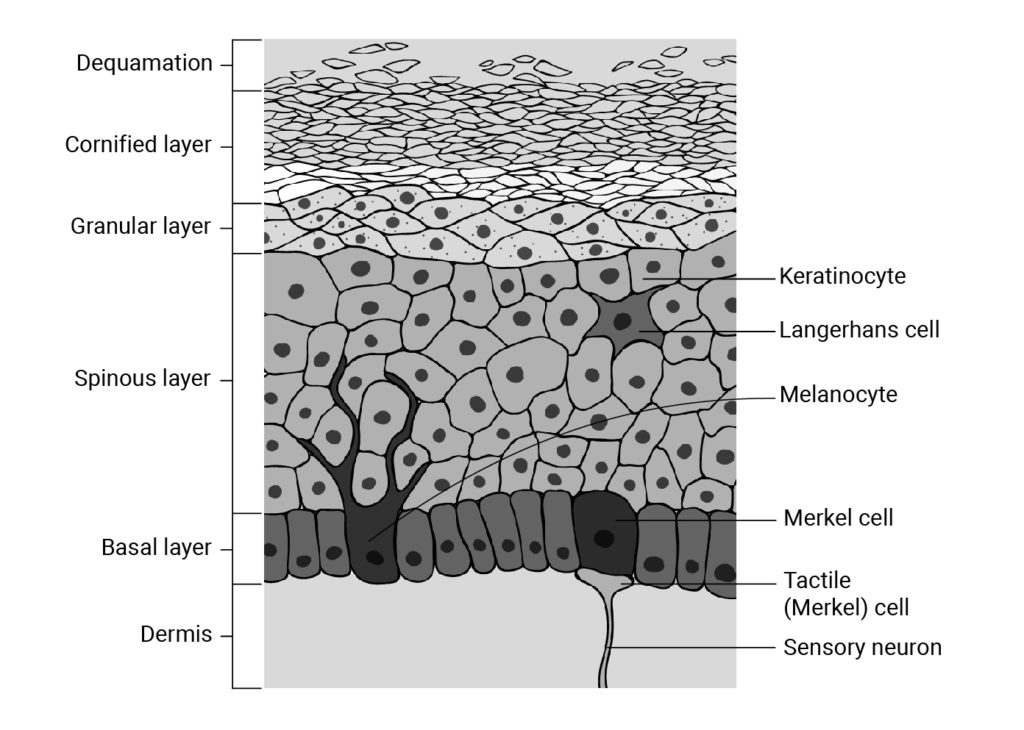
Figure: the layers of the epidermis. Conversion of 7-dehydrocholesterol to pre-vitamin D3 by a photoreaction promoted by UV-B occurs mostly in the basal and spinous layers of the epidermis. Illustration by Magda Levy.
Cutaneously synthesized vitamin D3 is released from the plasma membrane and enters the systemic circulation bound to vitamin D-binding protein. As a lipid-soluble molecule, vitamin D3 can be taken up by adipocytes and stored in subcutaneous fat for later use. Once in the circulation, vitamin D is converted first in the liver and then in the kidney to its active hormonal form, 1,25-dihydroxyvitamin D [1,25(OH)2D].
Skin color and vitamin D
Through evolution, northern latitudes selected for lighter skin that allows UV rays to produce vitamin D from 7-dehydrocholesterol. Conversely, latitudes near the equator selected for darker skin that can block a large portion of UV radiation. The lack of “adjustment” between where our ancestors lived and where we live now results in a Vitamin D insufficiency that affects almost 50% of the population worldwide. In any case, city life (and quarantines!) does not allow for much exposure to UV radiation whatever the color of our skin.
Vitamin D in skin differentiation and proliferation
Calcium and 1,25(OH)2D interact to regulate the skin differentiation process. 1,25(OH)2D increases the expression of involucrin, transglutaminase, loricrin, and filaggrin and increases the formation of the keratinocyte’s cornified envelope. The mechanism of action involves 1,25(OH)2D increasing intracellular calcium levels through the induction of the calcium receptor.
Cutaneous antimicrobial effects
1,25(OH)2D and its receptor regulate the processing of the long-chain glycosylceramides that are critical for the skin barrier formation, crucial in defending the skin. The pair also induces toll-like receptors that initiate the innate immune response in the skin. Long ago cod liver oil (rich in Vitamin D) was used as a treatment for tuberculosis. Vitamin D also influences innate immune responses to pathogens through the synthesis of antibacterial peptides called cathelicidins, and the antigen “presentation” by macrophages or dendritic cells.
Dietary sources and supplements
Vitamin D is available in 2 distinct forms, ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3). Sunshine exposure provides D3, while dietary sources are able to provide both forms.
Many factors affecting vitamin D production in the skin, including age, obesity, skin color, clothing habits, and sun avoidance practices have a strong impact on vitamin D synthesis. Sub-optimal vitamin D may be so common that it may end up being the “normal” state. Should you worry about Vitamin D? Maybe, if you have skin problems like atopic dermatitis, vitiligo, or frequent skin infections.
Dunn, P. M. (1998). Francis Glisson (1597-1677) and the “discovery” of rickets. Archives of Disease in Childhood – Fetal and Neonatal Edition, 78(2), F154–F155. doi:10.1136/fn.78.2.f154
Nair, R., & Maseeh, A. (2012). Vitamin D: The “sunshine” vitamin. Journal of pharmacology & pharmacotherapeutics, 3(2), 118–126. https://doi.org/10.4103/0976-500X.95506
DISCLAIMER: These claims have not been evaluated by the FDA and are not intended to diagnose, cure, treat, or prevent any disease.