The skin: layers of complexity and chemistry
Our skin is a protector against water loss to the environment and physical, chemical, and biological attack. To be able to do its job, the skin must be resistant to diverse agents. Live cells are too fragile to do that job, so the cells have to die, and they do that in a programmed sequence that involves massive biochemical and structural transformations. 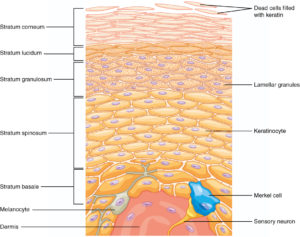
Figure: The epidermis: skin cells change shape and structure to form the different layers of the skin. Cornified cells (corneocytes) are dead cells, but they make up a layer (horny layer, stratum corneum in Latin) that prevents water loss and the entry of microbes.
Let’s start with the basal layer, the deepest layer of the epidermis. The basal (germinative) layer is a single row of cuboidal cells with large nuclei. Some of these basal cells have stem cell capacity and will divide and produce new cells. In the basal layer you will also find melanocytes, Langerhans and Merkel cells (touch receptors).
Melanocytes are cells present in the epidermis and hair follicles of human skin. These melanocytes are very different from the rest of the cells in the epidermis, and that is not surprising, as they arise from another part of the embryo, the neural crest cells. Melanocytes have enzymes that make melanin within specialized organelles named melanosomes. Melanocytes use dendrites to transfer the pigment parcels to the keratinocytes, where the melanin will form the caps that protect the DNA from UV damage.
The basal keratinocytes divide and form the keranocytes of the granular layer. The aspect of the cells and the biochemistry changes, as the synthesis of fibrillar proteins starts the process of keratinization . In the next layer, the granular cells make histidine- and cysteine-rich proteins that bind the keratin filaments together. They also secrete lipids and proteins to the intercellular space that will allow the skin to become a barrier to water loss. The cells lose the nuclei and become the dead cells that make up the horny layer.
The skin works because of the close interactions between cells, both physical (desmosomes) and chemical. How good is the skin in its protective job? Very good, when it’s healthy. The horny layer is a compact wall made of corneocytes and unique fat molecules. The corneocytes are the bricks and the intercellular lipids, which include ceramides, and proteins are the mortar. The horny layer, without live cells, is the protective barrier that allows the rest of the skin to do its job. Preventing trans-epidermal (through-the-skin), water loss (TEWL) is one of the main functions of the horny layer. Together with cholesterol and saturated fatty acids, ceramide creates a water-impermeable, protective coating to prevent excessive water loss due to evaporation, as well as a barrier against the entry of microorganisms.
The horny layer has no live cells but is biochemically active. The components of the natural moisturizing factor (NMF) present in this layer are breakdown products from the proteolysis of the filaggrin protein. The upper layer is rich in natural moisturizing factor (NMF), a mixture of amino acids and derivatives with a high binding capacity for water. NMF keeps the skin hydrated, but you can decrease this pool with frequent washing.
It is worth noting that some ingredients used in the skincare industry, like ceramides and sodium PCA, are chosen from those present naturally in the skin. It makes sense to start taking care of your skin by avoiding routines that remove these natural components. Preserving the natural components that make the skin a barrier will go a long way in preventing “sensitive skin,” a problem created by the skincare industry.
Next step? Desquamation.
What lies beneath the epidermis? Dermis and hypodermis
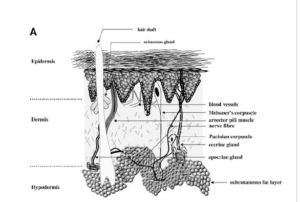
Figure: The skin, from top to bottom, epidermis, dermis, and hypodermis
We only see the very top layer of the skin, the dead cells of the epidermis. Below, the dermis and underlying tissue affect the shape of our face and the overall appearance of the skin.
A lot happens in the dermis, even when there aren’t many cells but mostly extracellular matrix (ECM), which anchors the cells. ECM is a complex component that influences cell survival, proliferation, and function. The cells are fibroblasts, a very adaptable type of cell that alters their biochemistry and physiology depending on where it is.
In the dermis, you will also find blood vessels, nerves, muscle fibers that can erect the fine hairs that traverse the kin, oil glands, sweat (apocrine) glands, Pacinian corpuscles. And more.
Elastin, collagen, proteoglycans and glycosaminoglycans, all of them are made in the dermis, where the fibroblasts are a factory of macromolecules. The synthesis starts within the fibroblast, but there is a lot of modification and assembly happening in the intercellular matrix. Signals come and go, and intercellular space and cells interact, and they also interact with the rest of the body via growth factors, hormones, nutrients. When our skin is damaged, and this happens all the time, repair requires the collaboration of the whole system. Resistance to invaders, bacteria or viruses, involves the activity of the immune system, the local one which includes Langerhans cells, and the cells and antibodies that come to the rescue from further away. Some glycoproteins, e.g., fibulins, become incorporated into the fibrillar extracellular matrix Fibulins have overlapping binding sites for several basement-membrane proteins, tropoelastin, fibrillin, fibronectin, and proteoglycans, and they participate in diverse supramolecular structures. Another glycoprotein, decorin, binds to collagen I fibrils and influences the assemblage of the ECM.
Below the dermis, the subcutaneous white adipose tissue (sWAT) may look well protected by epidermis and dermis, but it is also affected by the environment and aging. Why does it matter?
Changes in sWAT, including properties of the adipocytes in it, will affect skin resistance to mechanical stress and manifest as wrinkles. When people complain about their skin, they are often referring to changes concerning sWAT and the adhesion between skin and sWAT.
Why am I giving so much detail here? It is relevant to skincare: once you understand the complexity of the biology and biochemistry of the skin, it becomes evident that there can’t be a magic ingredient that will solve all the skin problems. Yes, vitamin C may affect the redox state of the skin, but it is no miracle ingredient. Conversely, it is possible to mess up this complex system with relative ease. Add too much copper, and a cascade of events will ensue.
Tracy, L. E., Minasian, R. A., & Caterson, E. J. (2016). Extracellular Matrix and Dermal Fibroblast Function in the Healing Wound. Advances in Wound Care, 5(3), 119–136. doi:10.1089/wound.2014.0561
Wollina, U., Wetzker, R., Abdel-Naser, M. B., & Kruglikov, I. L. (2017). Role of adipose tissue in facial aging. Clinical Interventions in Aging, Volume 12, 2069–2076. doi:10.2147/cia.s151599