Hyperpigmentation
The basics
The color of our skin is partly due to the pigment called melanin. Other factors are the content of diet carotenoids, the bluish-white color of connective tissue, and the abundance of blood vessels in the dermis and the color of blood flowing in them (oxy- and deoxy-hemoglobin). Other minor pigments (minor unless you have a bruise) are bilirubin (the yellow hemoglobin degradation product that colors bruises) and the complete sequence, which includes hemoglobin to biliverdin to bilirubin to hemosiderin. The different skin colors among individuals and races do not reflect major variation in numbers or size of melanocytes, but rather different kinds and amounts of melanin produced by the melanocytes. There are about 150 genes involved in the regulation of skin color in mice, including transcription factors, membrane proteins, enzymes, and several kinds of receptors and their ligands, and it is likely that these genes are still relevant in humans. This complexity, plus the troubled relationship of humans with skin color, explains the many inconsistencies I have seen in the scientific (and not so scientific) literature on the issue.
The color of our skin has been a major factor in inter-human relationships (and fodder for racists) for millennia, but the pigments have an actual physiological role: protection from UV light. Melanin absorbs UV across a wide spectrum, with the highest absorption in the shorter wavelengths that are most associated with DNA damage from UV.
UV light reaches human skin and leads to inflammation, DNA mutations, and more. Reactive oxygen species (ROS*) are induced in the skin by solar UVA and UVB radiation and have long been suspected of contributing to the deleterious effects of skin damage by sunlight. ROS* promote lipid peroxidation, protein oxidation and cross-linking, enzyme inactivation, and DNA damage. For example, singlet oxygen mediates the UVA induction of inflammatory cytokines which, in turn, increase collagenase (a protease that breaks down collagen) in the skin. These effects of ROS* result in decreased cell viability and biological function, increased degradation of the dermal extracellular matrix, skin carcinogenesis, and aging.
Skin pigmentation and cultures old and new
Evolution favored the accumulation of more and darker melanin in the skin of humans living near the equator, where UV radiation is much higher than nearer the poles. Brown or black skin protects against high levels of exposure to the sun, while sun exposure more commonly results in melanomas in lighter-skinned people. Melanin in the iris and choroid of the eyes helps protect them from UV and high energy visible light; therefore, people with light colored eyes are at higher risk for sun-related eye problems, like cataracts.
Melanin is a good response to UV, and it is inducible by it, the response we call “tanning”. In Europe, tanned skin was a sign of lower class, because people working in the fields were tanned and the owners of the fields were not. Conversely, in the 1950s tanning became fashionable, so the tan was still a class indicator but in the opposite direction. I hope that in the near future it will become fashionable to have non-tanned skin again.
In many cultures and countries lighter skin is still an indicator of class and, because of this, skin lightening is a billion dollar industry. In fact, many people risk their health for the promise of lighter skin; there are plenty of examples of dangerous chemicals and finished products used for skin lightening.
On the other hand, skin brightening is also important to people who develop uneven pigmentation, like melasma, which pushes them to try risky remedies. For example, chemical peels and laser may cause further hyperpigmentation in people with darker skin. This is why we feel it is important that we have healthy and safe ways to control pigmentation.
Main causes of uneven pigmentation
Aging: With skin aging comes dark (a.k.a. age, liver, or sun) spots, but also areas with loss of pigmentation. This is because mutations (caused by UV) in some areas lead to excess melanin production and accumulation, but in other areas melanocytes may have been lost or damaged.
Melasma: Genetics, visible light, UV, hormonal changes, and laser treatment all affect melasma. The hormonal influence, via pregnancy or by birth control pills, may be weaker than previously thought. Melasma is often inherited and even visible light appears to affect melasma. Apparently there is more than just melanin involved, as vascularity increases in areas of melasma. It is interesting that tranexamic acid, a medication used to control blood coagulation, seems to help with melasma. Unfortunately, long-term use of this drug is dangerous, as is often the case with drugs that affect several aspects of human metabolism.
Post-inflammatory pigmentation: Acne sufferers are familiar with this problem, but some “home remedies” tried by melasma sufferers may also cause hypepigmentation, because heating, laser, and peels all lead to stress and inflammation. Endothelin 1 (ET-1) is produced by keratinocytes after exposure to inflammatory stimuli or UV exposure and it stimulates melanogenesis.
Vitiligo: This is a condition that causes loss of pigmentation in sections of skin. It occurs when melanocytes die or are unable to function. The cause of vitiligo is unknown, but autoimmune mechanisms, oxidative stress, and viruses may be involved. For this particular skin problem, we suggest our Anti-Inflammatory Cream, Antioxidant Day Cream, and Antioxidant Serum.
Dark under-eye circles a.k.a. periocular pigmentation: Causes of dark under-eye pigmentation vary widely, but research suggests that the most common forms are:
1) the vascular type – characterized by the presence of redness (erythema) and involving inner aspects of lower eyelids with prominent capillaries/telangiectasia or bluish discoloration due to visible blue veins;
2) a constitutional form – characterized by the presence of brown-black hyperpigmentation of the lower eyelid skin along the shape of the orbital rim;
3) post-inflammatory hyperpigmentation – usually caused by allergic contact dermatitis; and
4) shadow effects due to an overhanging tarsal muscle or deep tear trough.
Other causes may include skin laxity, dry skin, hormonal disturbances, nutritional deficiencies, and chronic illnesses.
What to do? The Skin Actives Way
Dermatologists will usually indicate the triad of hydroquinone, retinoids, and corticosteroids. We at SAS like retinoids too, but our Vitamin A Cream is non-irritating. For anti-inflammatory activity we don’t use corticosteroids, and we don’t use hydroquinone. By keeping up with the scientific research, we can introduce promising new skin lightening ingredients that are also safe; like soy protease inhibitor, salicin, GSH, carotenoids, baicalein, and more. We are now introducing our new, updated Skin Brightening Cream.
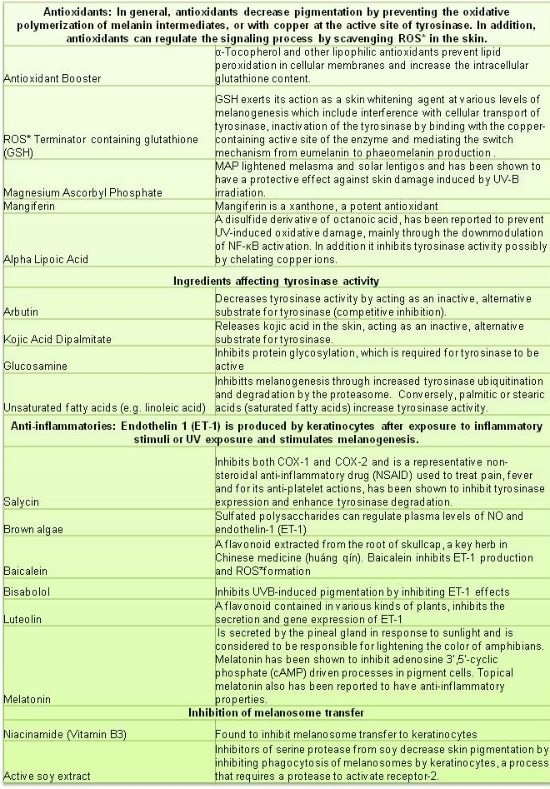
Our new Skin Brightening Cream seeks to address the multiple ways that pigmentation problems can occur. Active ingredients were chosen for the following reasons:
Because melanin synthesis increases as a response to stress of several kinds, like UV and oxidants, it is a good idea to avoid the sun and use sun block. In the case of melasma, it seems that visible light (not only UV) may have some influence, so it is best to use a physical sunscreen (one containing zinc oxide). You should also know that skin lighteners will not destroy existing melanin, so you will have to wait until your skin renews itself to be able to see the lighter skin.
What NOT to do?
Skin lighteners, skin whiteners, and skin brighteners are different names given to a type of product that decreases skin pigmentation. There are two kinds of people looking for skin lighteners; those with irregular pigmentation resulting from age spots and/or melasma, and those who are not content with the color of their skin. There are several mechanisms by which a substance can help to lighten the skin color, but most of them work by suppressing melanin synthesis. Some chemicals are very effective but can be irritating or are known to have undesirable side effects. For example, strong chemicals may end up bleaching the skin permanently and irregularly, or increasing pigmentation in spots. It is very important to avoid bad results. The best way is to not use strong chemicals like hydroquinone, especially in types of skin known to react badly, like African American and dark Latino skin.
What we want from our ingredients is specificity, and effect restricted to the area of application. One big problem with treatment of skin hyperpigmentation is that we humans are always looking for fast, easy, miraculous solutions. You will not get this with skin lighteners of uncertain origin. Illegal and restricted substances are often present in cosmetics sold for skin bleaching, in particular hydroquinone, tretinoin, and corticosteroids. In Belgium, 60% of skin whitening cosmetics were found to contain illegal substances, like clobetasol propionate and hydroquinone.
TGF-beta-1
Melanosomes are specialized organelles in which melanin is synthesized and deposited. The addition of TGF-β1 to cultured melanocytes produced less pigmented melanosomes even when the cells were concomitantly treated with αMSH to increase their fully melanized melanosomes. However, TGF-beta 1 is not a good candidate for skin lightening because of its multiple effects. TGF-beta 1 is a multifunctional peptide that controls proliferation, differentiation, and other functions in many cell types. TGF-β1 plays an important role in controlling the immune system, and has different effects on different types of cells, and even on cells at different developmental stages.
Topical corticosteroids
Topical corticosteroids have strong anti-inflammatory effects. They have been used for the treatment of melasma to decrease irritation caused by hypo-pigmenting agents and work by suppressing cytokines through the inhibition of nuclear factor kappa B (NF-κB) activation. Topical steroids can be effective by the suppression of cytokines such as endothelin-1 and GM-CSF, which mediate UV-induced pigmentation. Unfortunately, they can only be used short-term because of the numerous side effects.
Tranexamic acid
Tranexamic acid (trans-4-aminomethyl cyclohexane carboxylic acid) is a plasmin inhibitor commonly used as a haemostatic agent owing to its antifibrolytic action, and is also promoted as a systemic skin whitening agent especially as oral or intradermal injections for melasma. It is a synthetic derivative of lysine. Plasmin is a protease that enhances the intracellular release of arachidonic acid, a precursor of prostanoid, and also elevates alpha-melanocyte stimulating hormone (α-MSH) processed from pro-opio-melanocortin. Both arachidonic acid and α-MSH can activate melanin synthesis by melanocytes. Tranexamic acid, by way of its antiplasmin activity, depletes the keratinocyte pool of arachidonic acid involved in ultraviolet (UV) induced melanogenesis. It is not safe to use it for a long duration in view of its anti-hemorrhagic property resulting in side effects like venous thromboembolism, myocardial infarction, cerebrovascular accidents, and pulmonary embolism.
Another major question is whether switching, long-term, the normal machinery from eumelanin (which is protective against UV radiation) to pheomelanin (it has been suggested that this form favors UV-induced DNA damage) by an external agent like tranexamic acid, could result in an increased incidence of skin cancers.
Hydroquinone
Hydroquinone has been used for decades as a skin lightening agent, but mid-term effects (i.e. in a matter of months) are worrying. In about 70% of the users, there is deposition of yellow-brown pigment in the dermis, in addition to break-down of collagen and elastin. The chemical composition of the ochronotic material and the mechanism by which hydroquinone promotes its formation are unknown. Hydroquinone may also cause skin and renal cancer.