Eczema/atopic dermatitis update 2022.
Atopic dermatitis (AD, eczema is one of its forms) is a common, chronic inflammatory skin disease characterized by skin barrier dysfunction, inflammation, and itch. The exact mechanisms behind the pathogenesis of AD are very complex and still being studied, but we know that its development and persistence require interaction between skin barrier dysfunction, inflammation, and itch.
Eczema is a complex, multifaceted skin condition that has a strong genetic component. More than 30 genes have already been identified as implicated in eczema. Knowing the genes involved is not enough to understand the mechanisms involved but progress is being made all the time
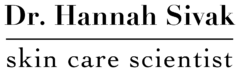
How does it start? It seems that abnormalities in skin components like filaggrin and intercellular lipids cause the disruption of the skin barrier, leading to the production of cytokines like interleukins that promote skin inflammation. Inflammation, in turn, suppresses the expression of filaggrin in keratinocytes and exacerbates epidermal barrier dysfunction. Inflammation will also lead to the production of itch mediators that will act on sensory nerves and cause itch.
In short, the three factors of AD are barrier dysfunction, skin inflammation, and itch. Management of atopic dermatitis requires control of the three components.
A new class of prescription medicines has been approved by the FDA to treat eczema: JAK inhibitors. This is a good time to review what we know about eczema and the new medication and answer a crucial question: is there still a place for Skin Actives anti-inflammatory cream, ELS serum, and our new ingredients?
From my book
Eczema and atopic dermatitis
We need our immune system to defend us from the infectious agents trying to invade us, like bacteria, viruses, or fungi. Sometimes the immune system does not work as well as we would like it to, and it plays tricks on us.The terms eczema, atopic dermatitis, and atopic eczema describe a chronic inflammatory skin disease with allergic causes. The skin itches, and there may be scales, crusting, and oozing (rather than just erythema or inflammation). Skin affected by eczema is more prone to bacterial infection because the skin barrier breaks, facilitating attack by microorganisms.
People who have eczema also tend to have other manifestations of allergy, like allergic rhinitis or asthma. Atopic dermatitis is widespread, affecting about 10% of the population, and it can start as early as two months of age.
Some characteristics of atopy (manifestations of a “skewed” immune system) are high concentrations of serum immunoglobulin E (IgE) and increased incidence of IgE-mediated responses (seen on skin testing) to common inhaled antigens.
What can you do if you or a loved one has atopic dermatitis? Avoid common allergens such as dust mites, animal dander and saliva, mold, and pollen. Children can have food allergies, so it is worth exploring this aspect with an MD’s help, always remembering that “exclusion diets” can deprive the child of essential nutrients (it happens frequently enough with adults).
Something that doesn’t seem to work for atopic dermatitis is immunotherapy (allergy shots), a practice that works for patients with asthma or rhinitis caused by allergens like pollen and dust mites.
Avoid factors that may worsen atopic dermatitis: excessive bathing, low humidity environments, emotional stress, dry skin, rapid temperature changes, and exposure to solvents and detergents. Doctors disagree on whether showering or bathing is preferable in patients with atopic dermatitis. Some doctors recommend a hydrating bath followed by immediate application of emollients. Others suggest a shower of short duration, which better removes surface antigens that may trigger an allergy.
The itchiness of eczema leads to scratching, and scratching leads to rashes. We need to stop this vicious circle because scratching can lead to permanent skin changes, including scars and infections. In an emergency, you can use hydrocortisone cream, but its long-term its use may lead to skin thinning, depigmentation and stretch marks. Also, corticosteroids will reach the bloodstream, suppressing the activity of the adrenal glands. Some over-the-counter (OTC) medications, like loratadine, work well for itching.
Evaporation of skin humidity leads to dry skin in patients with atopic dermatitis, and this is why skin hydration is a crucial component of overall management. Lotions have high water and low oil content and can worsen dry skin via evaporation, thus triggering eczema flares. Conversely, thick creams with low water content, or ointments, which have zero water content, protect the skin better against dryness (and eczema flares). Apply emollients like rosehip oil immediately after bathing to keep the skin well hydrated. Don’t ignore allergens present in “skincare” products like tea tree essential oil and cloth washing detergents containing enzymes. One of the saddest (horrifying) things in the industry is a diaper rash product containing a fragrance banned in Europe, Balsam of Peru, and a baby’s bottom affected by that product. Balsam of Peru contains many different chemicals, including cinnamic acid, cinnamyl cinnamate, benzyl benzoate, benzoic acid, cinnamyl alcohol, cinnamaldehyde, farnesol, and nerolidol. Is natural better? I don’t think so.
To alleviate the itching, you can use Skin Actives Scientific Sea Kelp Coral, calamine, rosehip, or pomegranate seed oil, or take a warm bath with oat beta-glucan, rosehip seed oil. Many actives seem to help with eczema; please have a look at our glossary.
Cannabidiol (CBD) binds to skin receptors involved in itching; oils with added CBD can help stop the itch-scratch cycles before the skin is damaged.
Eczema: a 2022 update
The only major change since the second edition of my book was published (2021) is that the FDA (USA Food and Drug Administration) has approved a new type of medication, a JAK inhibitor, for the treatment of atopic dermatitis. This is an addition to the many medications, old and new, that address the immune system disfunction that occurs in AD. As always, new medications come with their own limitations and side effects.
More medications that target the immune system will be added in the future, but topical skincare will still be needed. Why? Because management of atopic dermatitis, a complex skin problem, requires a multipronged approach.
Disruption of the skin barrier
What causes skin barrier dysfunction in people with AD? Mutations in genes relevant to the skin barrier, including filaggrin, proteins involved in the tight junction, production of lipids, will result in dry skin, increased trans-epidermal water loss, and ineffective skin barrier, allowing allergens to penetrate and sensitize immune cells in the skin. On top of this genetic predisposition, the use of detergents and alcohol in soaps, bubble bath, cleansers, etc., removed the skin components that protect the skin from trans-epidermal water loss and entry of irritants and infectious agents. In short, topical products often aggravate a predisposition to AD.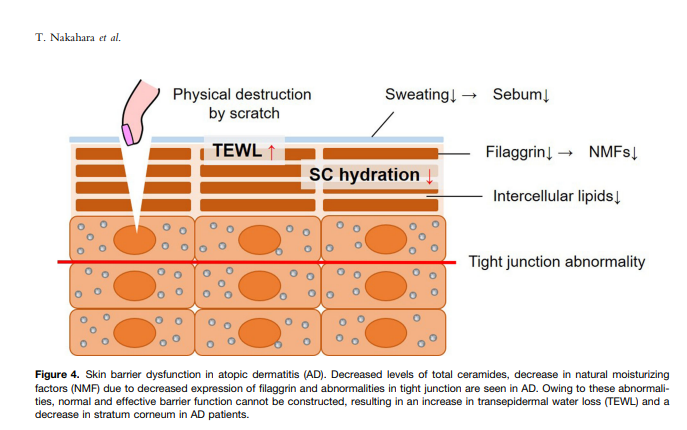
Figure: Skin barrier dysfunction from Nakahara et al., 2020 (see references).
The role of the yeast Malassezia
The broken skin barrier is a point of entry for infectious agents and causes an imbalance in the natural skin microbiological flora, with commensal bacteria and yeasts overcoming skin defenses. The yeast Malassezia is likely an opportunistic invader of eczema skin, but it can become an aggravating factor. The interaction between Malassezia spp. and the skin immune system contributes to skin inflammation in patients.
Cytokines in atopic dermatitis. JAK inhibitors
Because the skin is so important in keeping us safe from the environment, it has complex mechanisms to defend us from invaders like bacteria and fungi. These mechanisms go haywire in AD, just like they do in other manifestations of allergy. With the skin barrier damaged, allergens are able to interact with Langerhans cells and dendritic cells in the dermis. Immune activation of signal pathways leads to cell migration, production of various cytokines, hyperplasia, and other symptoms of AD. Some factors in the development of eczema.
Nuclear factor-kappa B (NF-κB) is an ancient (in evolutionary terms) protein transcription factor and is considered a regulator of innate immunity. The NF-κB signaling pathway links pathogenic signals and cellular danger signals thus organizing cellular resistance to invading pathogens. TH2 cytokines (IL-4 and IL-13) downregulate the production of filaggrin and keratins, reinforcing the AD cycle.
Figure: from Paller, A. S., Kabashima, K., & Bieber, T. (2017). Therapeutic pipeline for atopic dermatitis: End of the drought? Journal of Allergy and Clinical Immunology, 140(3), 633–643. doi:10.1016/j.jaci.2017.07.006
JAK inhibitors. What are they?
Phosphorylation of receptors by Janus kinases is just a part of this complex cascade of events, but one that is now being used as a therapeutic tool in immune-related illness. Various JAK-specific, small-molecule inhibitors are in clinical development for autoimmune disorders, including alopecia areata. These inhibitors can be extremely effective but side effects should be taken into account.
Upon interaction between a cytokine and a cytokine receptor, JAK kinases phosphorylate intracellular tyrosine residues on the cytoplasmic domain of cytokine receptors to initiate a cascade of signaling events: the JAK-STAT pathway (see figure below).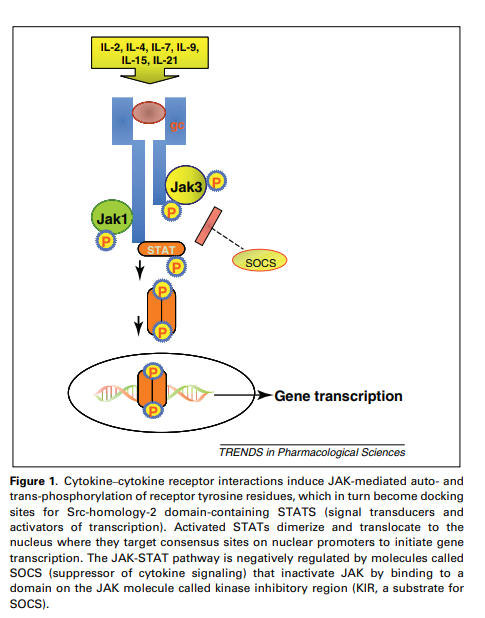
Figure: how JAK inhibitors interfere with signal transduction. From Vijayakrishnan, L., Venkataramanan, R., & Gulati, P. (2011).
Why itchy skin?
Itch is mediated by cutaneous sensory nerve fibers originating from cell bodies in the dorsal root ganglion, cluster of neurons in a dorsal root of a spinal nerve.. The free nerve endings exist in the epidermis, papillary dermis, and around skin appendages, and are activated by endogenous and exogenous pruritogens such as histamine, interleukin (IL)-31, thymic stromal lymphopoietin (TSLP), endothelin-1 (ET-1) and periostin through relevant receptors.
In AD, hyperinnervation may occur. Sensory nerve fibers may elongate in response to an imbalance between nerve growth factor (upregulated in AD), and inhibitors of nerve elongation. The threshold of excitability of nerve fibers may decrease and astrocytes, a form of glial cell, may change behavior, with activation of STAT3 (a transcription factor) leading to the production of lipocalin-2.
Main points
Controlling atopic dermatitis requires
• elimination of exacerbating factors,
• restoration of the skin barrier function
• hydration of the skin
• treatment of skin inflammation
• decreasing allergic reactions
• avoiding topical “natural” products that cause eczema because they are allergenic and disruptors of the skin barrier
Medication options (over-the-counter and prescription)
• Immunosuppressive drugs like glucocorticoids, work but have side effects
• Jak inhibitors oral JAK inhibitors (tofacitinib, abrocitinib, upadacitinib) may increase the risk of serious infections, major cardiovascular events (heart attack, stroke), cancer (lymphoma, lung cancer), thrombosis, and death.
• Calcineurin inhibitors
• Allergen immunotherapy: not very effective for AD
• Oral anti-allergics (Allegra, Zyrtec, etc.)
Steps to control eczema. In bold, are the steps that Skin Actives can contribute.
• Patch-up skin barrier disruption with topical occlusive products
• Keep the skin well hydrated
• Avoid further disruption: avoid bubble baths, alcohol, abrasion, and prevent scratching at all costs
• Avoid ingredients that are allergenic like some fragrances and tea tree oil. Unfortunately, some “natural” products supposedly formulated for sensitive skin, contain allergenic ingredients, practically ensuring that eczema will develop or worsen.
• Control opportunistic allergens like Malassezia with antifungals and pre-biotics (bee defensin, hops extract)
• Keep skin pH mildly acidic to prevent fungal growth
• Use plant extracts and pure chemicals that are known to interfere with the different steps in the development of AD
References
Glatz M, Bosshard PP, Hoetzenecker W, Schmid-Grendelmeier P. The Role of Malassezia spp. in Atopic Dermatitis. J Clin Med. 2015;4(6):1217-1228. Published 2015 May 29. doi:10.3390/jcm4061217
Grimm H, Mayer K, Mayser P, Eigenbrodt E. Regulatory potential of n-3 fatty acids in immunological and inflammatory processes. Br J Nutr. 2002 Jan;87 Suppl 1:S59-67. doi: 10.1079/bjn2001457. PMID: 11895155.
Kaczmarski, M., Cudowska, B., Sawicka-Żukowska, M., & Bobrus-Chociej, A. (2013). Supplementation with long chain polyunsaturated fatty acids in treatment of atopic dermatitis in children. Advances in Dermatology and Allergology, 2, 103–107. doi:10.5114/pdia.2013.34160
Kapur, S., Watson, W., & Carr, S. (2018). Atopic dermatitis. Allergy, Asthma & Clinical Immunology, 14(S2). doi:10.1186/s13223-018-0281-6
Maliyar, K., Sibbald, C., Pope, E., & Gary Sibbald, R. (2018). Diagnosis and Management of Atopic Dermatitis. Advances in Skin & Wound Care, 31(12), 538–550.
10.1097/01.ASW.0000547414.38888.8d
Nakahara, T., Kido‐Nakahara, M., Tsuji, G., & Furue, M. (2020). Basics and recent advances in the pathophysiology of atopic dermatitis. The Journal of Dermatology, 48(2), 130–139. doi:10.1111/1346-8138.15664
Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: End of the drought? J Allergy Clin Immunol. 2017 Sep;140(3):633-643. doi: 10.1016/j.jaci.2017.07.006. PMID: 28887947.
Panther DJ, Jacob SE. The Importance of Acidification in Atopic Eczema: An Underexplored Avenue for Treatment. J Clin Med. 2015;4(5):970-978. Published 2015 May 18. doi:10.3390/jcm4050970
Vijayakrishnan, L., Venkataramanan, R., & Gulati, P. (2011). Treating inflammation with the Janus Kinase inhibitor CP-690,550. Trends in Pharmacological Sciences, 32(1), 25–34. doi:10.1016/j.tips.2010.10.004
Zihni, C., Mills, C., Matter, K. et al. Tight junctions: from simple barriers to multifunctional molecular gates. Nat Rev Mol Cell Biol 17, 564–580 (2016). https://doi.org/10.1038/nrm.2016.80
DISCLAIMER: These claims have not been evaluated by the FDA and are not intended to diagnose, cure, treat or prevent any disease.